4 May 2022
Anaesthesia and analgesia for patients with cancer
Collette Dempsey and Miguel Martinez argue for the consideration of these processes when treating cancer in pets.

Since the start of the pandemic in 2020, the Pet Food Manufacturers’ Association estimates that 3.2 million UK households acquired a new pet. In the UK, approximately 59% of households own a pet, with the most popular pet type being a dog.
According to the Association of British Insurers, 4.8 million pets in the UK are insured, of which 2.8 million are dogs, 1.3 million cats and 700,000 others.
The American Veterinary Medical Association estimated that approximately one in four dogs will, at some stage in their life, develop neoplasia. Almost half of dogs over the age of 10 will develop cancer. Dogs get cancer at roughly the same rate as humans, while less information exists about the rate of cancer in cats.
These statistics will prompt increased pressure on the UK veterinary industry now and in the future to treat more pets developing cancer.

When treating cancer in our patients, we often think of the surgical technique and chemotherapy options available. These options are numerous and will not be discussed in detail in this article. The aim of this work is to question if we give consideration to the anaesthetic techniques we use to allow for these treatments.
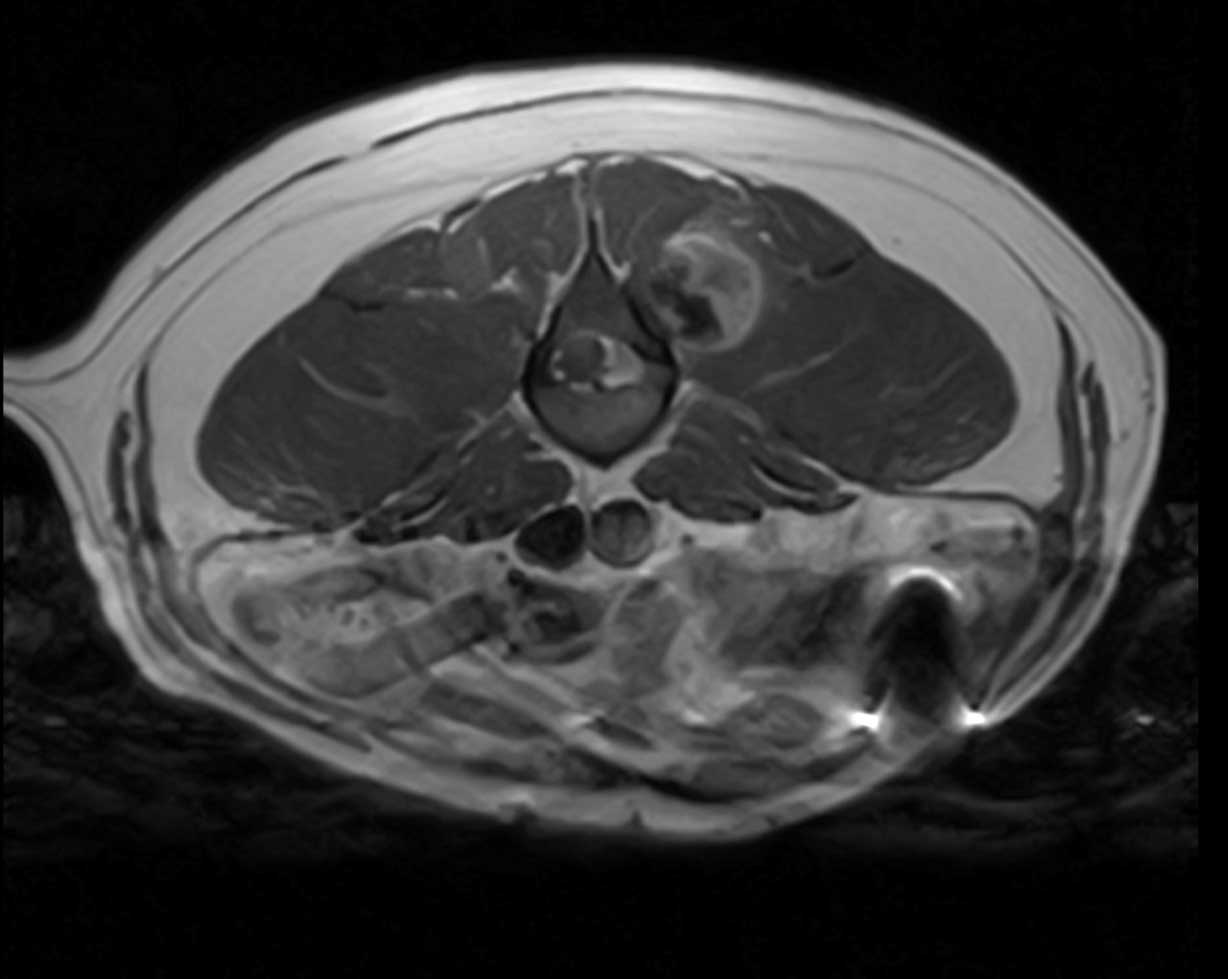
In human medicine, many protocols and procedures can be undertaken in a conscious state, but this is not often possible when treating animals. Diagnostic tests and treatments often require a degree of sedation or general anaesthesia.
The effects analgesia and anaesthetic agents have on the body systems, and the implications of these when cancer is present, poses the question: should we reconsider our approach to anaesthesia in cancer cases?
When planning for tumour removal, the surgeon will possibly complete a surgical request form. This details the kit list; whether assistance is required, possibly if antihistamine has been prescribed or not, surgical clip, antibiotic prescription, and other important instructions.
The aim of this article would be to open the idea to add anaesthetic considerations to this list. Some practices would have protocols developed for routine surgeries. In an ideal world, we should assess every individual and tailor each patient’s anaesthetic plan to the individual’s health status and the procedure taking place.
Anaesthesia
Anaesthesia is a state of controlled, temporary loss of consciousness and mobility. The drugs used affect the body systems; apart from the desired effect of CNS, depression and unconsciousness, these can include inflammation, hypoxia, release of growth factors, angiogenesis and immunosuppression.
All of these can create an opportunistic environment for cancer cells to proliferate. The surgical insult and the anaesthetic agent will activate the neuroendocrine paracrine response, the hypothalamic-pituitary-adrenal axis (HPA-axis) and sympathetic nervous system (SNS) to work simultaneously.
The HPA-axis suppresses cell-mediated immunity (CMI) by decreasing the natural killer (NK) cell cytotoxicity and cytotoxic T-lymphocytes (CTLs), which would ordinarily combat the residual cancer cells.
The SNS releases catecholamines, cortisol, endogenous opioids and prostaglandins. The release of these will also affect the NK cells and CTLs. Together, these actions decrease interleukin-12 (IL-12), tumour necrosis factor (TNF-α) and interferon-y; this in turn alters the cytokine balance of T-helper 1 (TH-1) and T-helper 2 (TH-2), giving dominance to anti-CMI TH-21.
TH-2 cytokines accumulate arginase-1 expressing myeloid-derived suppressor cells (MDSCs) in lymphoid tissue. An arginine-deficient environment will result in a reduction of effective lymphocytes in circulation. The down-regulation of CMI increases MDSCs, transforming growth factor (TGF) and T-regulatory cells leading to immunosuppression. It has been suggested that tumour derived MDSCs inhibit NK cell activity by producing TGF-beta.
When the SNS releases the catecholamines and other soluble factors, this introduces tumour-associated macrophages (TAMs).
An increase in these various soluble factors allows for proinflammatory and anti-inflammatory responses and, in turn, angiogenesis to occur.
In the end, tumour angiogenesis and immunosuppression is the recipe for tumour progression or metastases from micro-metastasis or residual tumour cells from the primary tumour.

Stress
Stress-induced immunosuppression around the perioperative period is a perfect opportunity for tumour cells to disseminate.
It has been suggested that reduction of stress during the perioperative period will reduce immunosuppression, and, consequently, decrease the likelihood of tumour recurrence and further distant metastases. When creating an anaesthetic plan for a solid tumour removal, the anaesthetist should consider how to manage stress and pain to reduce immunosuppression. Simple environmental factors to reduce stress, such as a calm environment and handling of the patient, can help. Minimal handling of the actual solid tumour will prevent histamine release.
An effective premedication will allow a smooth anaesthetic induction and adequate analgesia for the surgery, as well as consideration of the anaesthetic drugs to be administered.
Inhalation
Inhalation anaesthesia, such as isoflurane, has been shown to increase hypoxia inducible factors (HIF); this is dependent on the duration of use and concentration.
The longer the exposure and the higher the concentration of isoflurane used, the greater the stimulation of HIFs. HIFs are a group of transcription factors that control the response to hypoxia. Hypoxia can result in angiogenesis and glycolysis, and this in turn promotes cell proliferation, which could be detrimental to our cancer patients.
Sevoflurane and desflurane have similar effects, so no one inhalation agent has been proved to be preferable. In vivo studies have concluded that clinically relevant concentrations of inhalation agents promote tumour growth in human prostate, ovarian, breast, neuroblastoma and lung cancer.
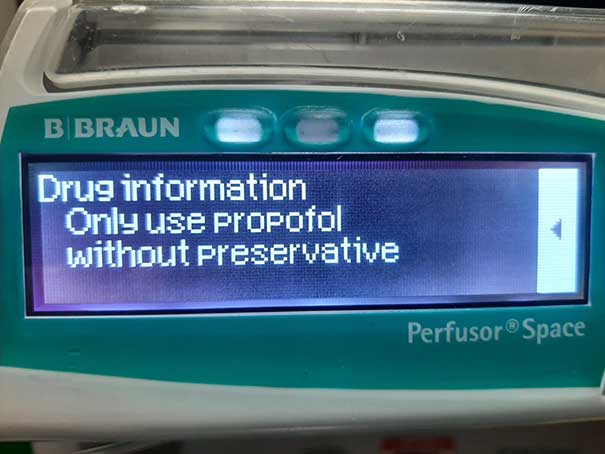
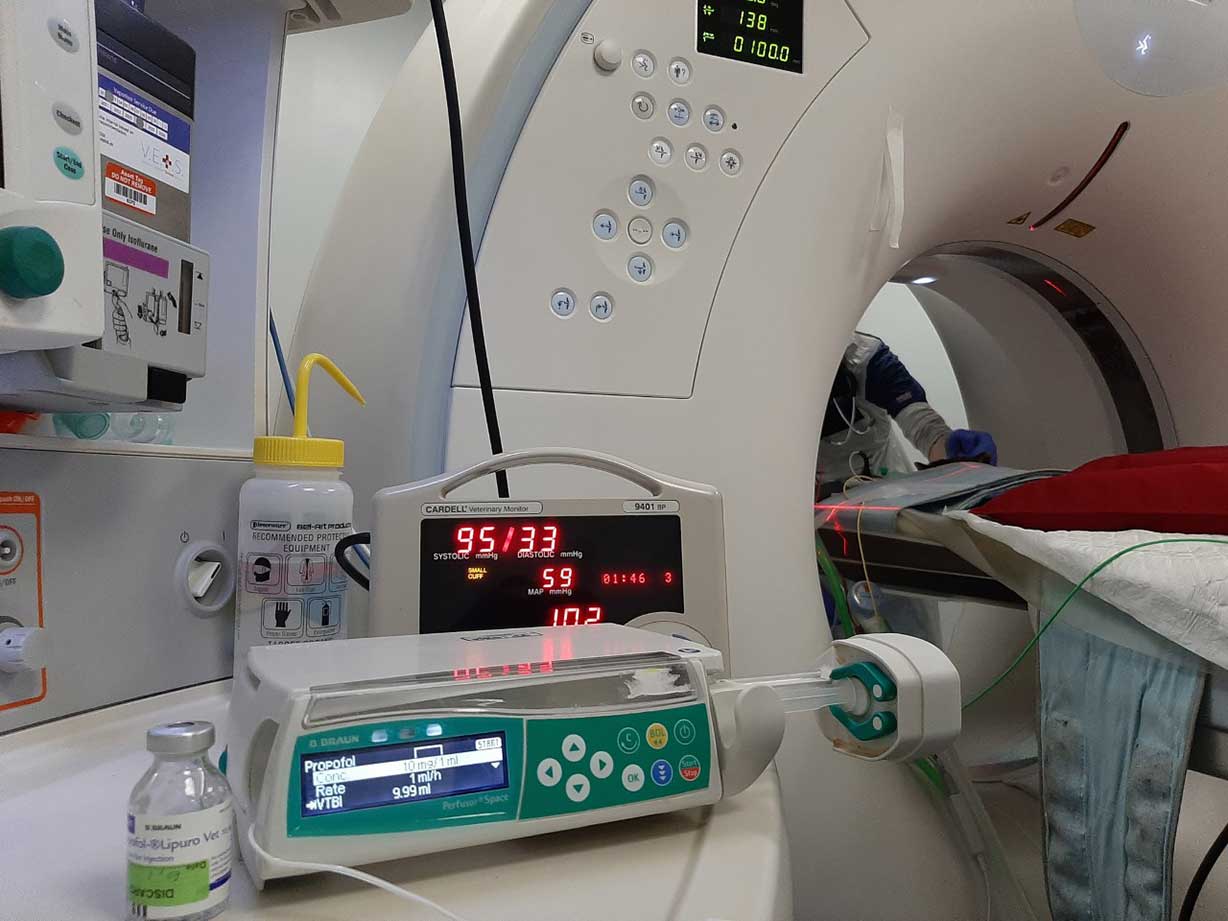
Anaesthetists can consider reducing the need for inhalation agents in a few ways (for example, loco-regional anaesthesia or total intravenous anaesthesia; TIVA). When considering TIVA, propofol has a number of beneficial effects. Propofol has been shown to stop ischaemic preconditioning in a trial with rat models reducing HIF-1α expression in a concentration/time-dependent manner2. Propofol has also been proven to increase apoptosis and preserves NK cell function.
Due to these findings, it is thought propofol inhibits tumour cell growth, hence it would be advantageous to use propofol for induction and maintenance of anaesthesia.
TIVA and regional anaesthesia has been shown to be the superior approach versus inhalation anaesthetic in a trial where a population was implanted with luciferase-tagged murine 4T1 breast cancer cells. Surgical dissection of the mammary tumour with sevoflurane had significantly more metastases than the group with propofol3.
Pain management
Management of pain in the immediate surgical scenario or in the postoperative phase is an important consideration in clinical oncology.
Pain management in oncology is a growing practice as understanding of the disease progression, clinical outcomes and the immune system improves. Pain itself is also immunosuppressive, and immunity is needed to protect against cancer cells.
Blocking the pain pathways with general anaesthetics, local/regional anaesthetics, analgesics, such as opioids, and anti-inflammatory drugs will help reduce the effect of the HPA axis.
Opioids
Opioids are a class of drugs that act on the opioid receptors. Like all drugs, opioids have desirable and undesirable effects.
The desired effect is analgesia. Undesirable effects can be bradycardia, reduced gut motility, nausea, and immunosuppression. Direct and indirect effects on the immune system are seen. Direct effects on the immune cells are manifested via opioid and non-opioid Toll-like receptors. Indirect effects are manifested via the SNS and HPA axis (Table 1).
| Table 1. Effects of opioids on the immune system | |||
|---|---|---|---|
| Opioid | Receptors acted on | Natural killer cell toxicity | Cancer cell |
| Morphine | μ-opioid peptide (MOP) | Decrease/no effect post-surgery | Increase |
| Methadone | MOP | Unknown; requires research | Unknown |
| Fentanyl | MOP | Decrease/no effect post-surgery | Increase |
| Buprenorphine | • MOP – partial agonist • kappa-opioid peptide antagonist |
No effect/reverse suppression post-surgery | No effect |
| Tramadol | MOP | Increase/reverse suppression post-surgery | Decrease |
Regional and local
Regional anaesthesia could be a useful tool in the anaesthesia plan. The neuraxial techniques (such as epidural) and the consequent sympathetic blockade will not only reduce the need for systemic opioid use perioperatively, but also avoid the potential detrimental effects of immunosuppression from these drugs.
This is theoretical and studies so far have not proven that regional anaesthesia has any anti-tumour effects, but the drugs we use in these techniques may be of interest. Local anaesthetics have been shown to inhibit the epidermal growth factor receptor4.
Another report explains how local anaesthetics down-regulate the nuclear factor kB (NF-kB)5.
This leads to the thought that local anaesthetics can have an immunomodulatory effect and could, therefore, potentially have a direct effect on cancer malignancies.
More research and clinical trials are needed to explore the use and effects of the local anaesthetics commonly used in veterinary nerve blocks. Effective regional anaesthesia will help enhance recovery after surgery.

NSAIDs
NSAIDs are common pain relief medication in practice. In fact, since their introduction into veterinary medicine, NSAIDs are the most prescribed medication in clinical practice.
NSAIDs’ mode of action is inhibition of cyclooxygenase 1 and 2. These enzymes catalyse the production of prostaglandins. The impact that prostaglandins have on the immune response favours the development and progression of neoplasia.
Prostaglandins have also shown to have a negative effect on NK cell cytotoxicity, cytokine secretion and migration, which further enables migrating cells to avoid the host’s immune response. In human medicine, it has been found that use of NSAIDs has even reduced the risk of developing cancer. In addition to reducing the risk of developing cancer, it has been shown in murine trials the NSAID celecoxib reduces angiogenesis and metastasis4.
Therefore, we can say with the absence of any evidence to the contrary that NSAIDs are beneficial in cancer patients, not only for multimodal analgesia, but also for their effects on cancer development or progression.
Recovery
In human medicine, enhanced recovery after surgery (ERAS) is a set of techniques commonly applied to patients in the perioperative period. When applied to our dogs and cats, we aim to reduce stress and pain and shorten the time to return to normal functions.
As we know, opioids can have detrimental effects on our patients. Hence reducing the need for opioids post-surgery would be beneficial.
We should always provide adequate analgesia, but we need to take into consideration the subsequent effects on the body.
It is interesting that not all opioids act in the same way. Morphine is thought to promote the development of cancer cells by decreasing NK cell cytotoxicity, but tramadol does the opposite by increasing the NK cell cytotoxicity; therefore, decreasing cancer cell development.
In human medicine, it is believed that minimisation of surgical stress and prompt return to normal function post-procedure improves short-term outcomes. A shorter post-surgical recovery time will be beneficial because it allows for earlier return to intended oncological therapy (RIOT); this in hand will maximise the overall success of treatment. It has even been suggested that RIOT-rate should be used as a quality measurement for surgical management. However, while the evidence is growing that ERAS and RIOT rate have impacts on overall success, the impact on the long-term mortality rate and disease-free survival will require more research and evidence to show this conclusively.
Unfortunately, studies so far have been retrospective. Several prospective studies have been planned and randomised clinical trials are underway, and in future these could give more definitive conclusions on the preferred anaesthetic techniques and prescriptions of analgesia.
When we have answers to these questions, veterinarians in practice can look to follow, advise and improve protocols.
