25 Jul 2023
Rhinoscopy for neoplasia debridement in a pet rabbit
Sergio Silvetti DVM, CertAVP(ZM), MRCVS and Lourdes Lavilla-Atienza MRCVS discuss retrograde rhinoscopy on a five-month-old miniature lop rabbit.

Image: © fotoparus / Adobe Stock
This case report describes the management of almost complete occlusion of the upper respiratory tract in a dwarf lop rabbit. The case was referred for investigation of ongoing respiratory problems unresponsive to the medical treatment. A CT scan revealed a polypoid mass extending from the skull base to the retropharyngeal space.
The approach chosen used a retropharyngeal endoscopic approach for a gross debulking of the mass to reduce restrictions to airflow, and for the collection of tissue biopsies to obtain an accurate prognosis. The incision area was easily identified with the help of the endoscope stylet inserted intraorally and pushed caudolaterally in the retropharyngeal tissues. The endoscopic debridement, performed with 5F semi-flexible biopsy forceps, achieved reduction of the airway narrowing satisfactorily in a short time with minimal bleeding. A total incisor extraction was performed concurrently due to co-existing malocclusion.
The histopathology identified an osteoblastic osteosarcoma, an uncommon neoplasia described in rabbits. Unfortunately, the rabbit developed fatal post-surgical complications which caused the death of the patient before any possible further intervention, and a necropsy was declined by the owner.
Despite the unfortunate outcome, the endoscopic approach of the retropharyngeal space revealed a valid approach to achieve full access of the pharyngeal space and the caudal nasal cavities space, not otherwise approachable with anterograde rhinoscopy; the approach was easy, with very limited haemorrhages and with no major visible vessels.
Respiratory conditions in rabbits are among the most common reasons for clinical presentation in daily practice, although a true prevalence of upper respiratory conditions in rabbits has not been determined (Benato et al, 2021).
Most of the upper respiratory conditions can present with similar signs despite the vast variety of aetiologies (Silvetti, 2021). A thorough investigation should be considered in every case of upper respiratory signs, with or without nasal discharge (Silvetti, 2021).
Neoplastic diseases in rabbits are commonly described as affecting the reproductive tract, with uterine adenocarcinoma the most common neoplasm, followed by lymphoma (Bertram et al, 2021; Baum, 2021).
Osteoblastic osteosarcoma is an uncommon neoplasia that, in rabbits, develops mainly in the skull (Zeeland, 2017; Bertram et al, 2021; Baum, 2021), while in dogs and cats, it is more commonly found on the limbs (Ehrhart et al, 2013). Metastases are very common, and 50% of the rabbits presented with signs of osteosarcoma have developed metastasis already (Zeeland, 2017).
Radiography, CT and rhinoscopy should be part of the routine diagnostic protocol in rabbit respiratory medicine (Eatwell, 2012). Anterograde rhinoscopy poses limits to the depth of possible investigation and collection of diagnostic samples, due to the size of the average patients seen in practice and because the size of the standard endoscopic equipment (Divers, 2010). Retrograde or retro-pharyngeal rhinoscopy is described for the access of the choana area and the space behind the soft palate to allow collection of biopsy samples in cats (Lhermette and Sobel, 2008a), where the anatomy of the area does not allow the use of a flexible endoscope commonly used in dogs (Lhermette and Sobel, 2008b).
Case report
A five-year and nine-month-old neutered female miniature lop rabbit was referred to investigate and treat respiratory problems that had started seven weeks prior to presentation.
The referring veterinarian started the patient with a course of 16 days of oral enrofloxacin and also performed a cheek teeth burring procedure after having found some dental malocclusion.
The rabbit seemed to improve after the procedure, but the respiratory signs did not fully improve. On clinical examination, the patient weight was 1.7kg; marked audible respiratory noise was evident, which worsened during and after handling for examination.
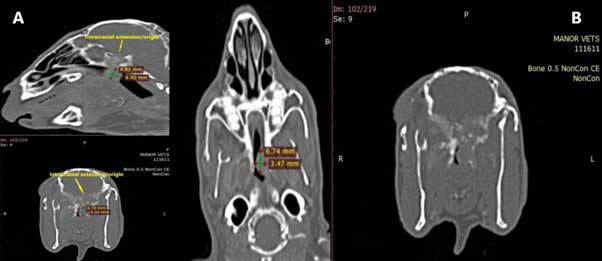
Incisor malocclusion and malocclusion of 308 with generalised elongation of the mandibular arcade teeth was also noted. A skull and thoracic CT scan was performed, with the patient sedated with intramuscular medetomidine (0.1mg/kg), midazolam (0.5mg/kg) and buprenorphine (0.06mg/kg), and after the procedure, a clinical crown reduction with occlusal surface reshaping and a reduction of incisor clinical crown length was performed at the same time.
The rabbit recovered uneventfully from the procedure and was discharged with oral meloxicam (0.5mg/kg every 12 hours).
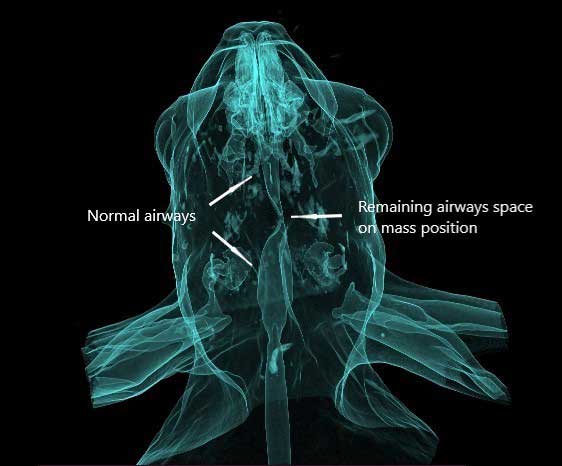
The CT report described an invasive nasopharyngeal polypoid mass with intracranial extension (Figure 1), dental disease with incisor malocclusion and clinical crowns elongation more pronounced on the left maxillary arcade (Figure 2); an incidental finding was a non-clinically significant right-sided otitis media and externa.

The CT findings were discussed in depth with the owner, including the limitations in access and treatment of the intracranial mass potential referral for radiotherapy, and the possible surgical approach to improve the airways of the patient, for which breathing conditions seemed to deteriorate.
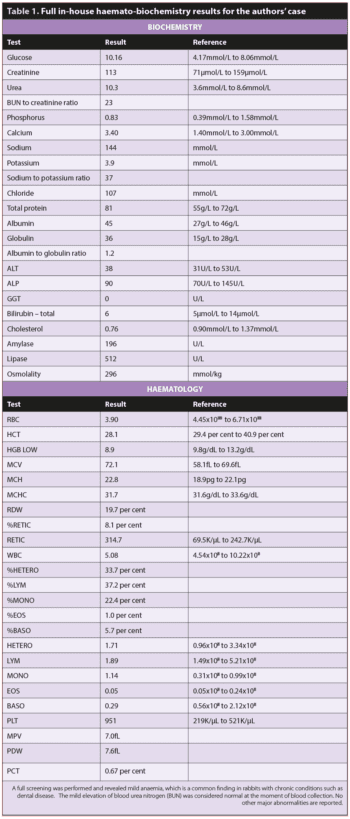
Before the procedure, a full in-house haemato-biochemistry screening was performed, revealing only mild anaemia – not uncommon in rabbits with chronic conditions (Varga, 2014) – but no biochemical abnormalities (Table 1).
The patient was premedicated with medetomidine 0.1mg/kg, methadone 0.5mg/kg and ketamine 5mg/kg, by intramuscular injection, followed by 0.5mg/kg of alfaxalone via intravenous catheter placed in the lateral ear vein.
The patient’s glottis was sprayed with local lidocaine solution and then intubated with a endotracheal tube size 3mm OD, and anaesthesia was maintained with isoflurane in oxygen 2% to 2.5%.
A sharp incision was made over the left retromandibular area, just caudally the mandibular ramus; the endoscopy stylet was used to highlight the area (Figure 3).
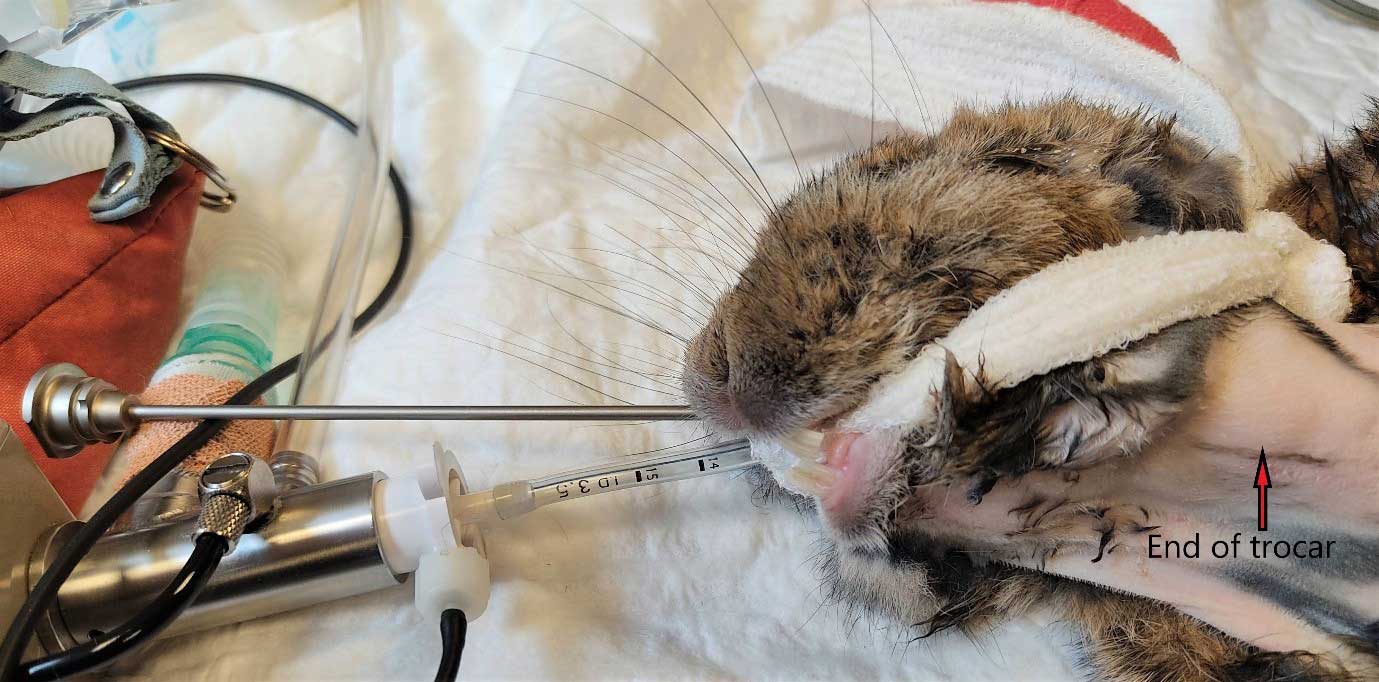
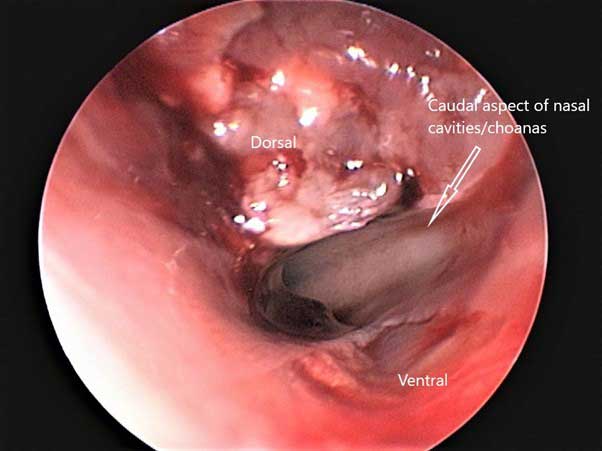
After the skin incision, a blunt dissection of the tissues allowed the identification of the major vessels. The soft tissues covering the tip of the stopcock were incised (Figure 4) and the 2.7mm with a 14F operative sheath that allows the use of 5F semi-flexible instruments (biopsy and grasping forceps, scissors) was inserted in the surgical wound; the retro-pharyngeal area was readily visualised, and the mass identified immediately (Figure 5).

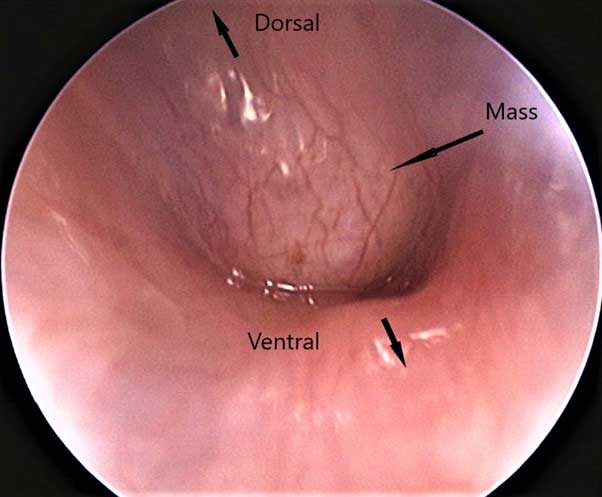
The debridement carried out with the biopsy forceps allowed a definite improvement of the airway size (Figure 6), and the collection of bacteriology and histopathology samples. Minimal haemorrhage occurred during the debridement, quickly controlled by sterile cotton bud pressure passed along the endoscope.
The incision was then sutured with poliglecaprone 50 4-0 in two layers, the first one of the pharyngeal tissues in a continuous introverting pattern, and the second one the skin with intracuticular continuous pattern.
The endoscopic procedure and the mass debridement lasted 25 minutes, and because the patient was very stable during the whole of the procedure, the incisor extraction requested by the owner was subsequently performed; the extractions were quick and uneventful.
The patient recovered from the anaesthesia very quickly; it was extubated five minutes after the end of the extraction procedure.
Once stable enough, a routine assisted feeding with Critical Care — Herbivore Recovery Food (Oxbow Animal Health) was started. The patient was discharged the same night with continuation of the already-started treatment and supplemental analgesia with oral compounded tramadol at 5mg/kg every 12 hours.
By 24 hours post-discharge, the owner reported by telephone that the patient started eating on its own and, despite being still weaker than normal, was bright and alert.
Unfortunately, the patient presented at the scheduled postoperative check-up 72 hours post-surgery alert, but not bright; an estimated dehydration degree of 5% was diagnosed, and a large and fluctuant swelling was present at the surgical area, from which several millilitres of green fluid with vegetable material was aspirated. Failure of the suture was suspected, and hospitalisation for fluid therapy and supportive care was recommended for a reviewing surgery, but it was declined by the owner, who preferred taking the rabbit home. The patient died the following morning on its way to the surgery for a corrective surgery. A full necropsy was declined.
The bacteriology received five days after the surgery of the mass was negative, no bacteria were isolated from the sample, and the histology, received seven days after the collection, reported findings according with spindle cell sarcoma, most consistent with osteoblastic osteosarcoma.
Discussion
The use of endoscopy has increased exponentially in recent years to improve the diagnostic and treatment options in the management of non-traditional companion animals (Divers, 2015a).
Smaller endoscopes with integrated operative sheaths allow investigations and improve diagnostics in very small animals (Divers, 2015a). In dogs and cats, the investigation of the retro-pharyngeal space and caudal nasal cavities can be achieved in two different ways: with a small flexible endoscope inserted through the oral cavity, or a rigid endoscope through the retro-mandibular access site (Lhermette and Sobel, 2008b).
In canine and feline medicine, the use of small flexible endoscope allows a non-invasive inspection of the retro-pharyngeal space and the most caudal aspect of the caudal nasal cavities (Lhermette and Sobel, 2008b).
Despite the more invasive procedure, retromandibular access with rigid endoscope allows a direct view of the field and the possibility of “deeper” penetration in the caudal nasal cavities (Lhermette and Sobel, 2008a). In dog and cat medicine, the retro-mandibular approach is used to identify and biopsy masses, collect cytological and bacteriology samples, to remove foreign bodies otherwise not accessible via anterograde rhinoscopy and to debride or debulk masses that occlude the airways (Lhermette and Sobel, 2008b).
In rabbit medicine, rhinoscopy is limited only on the anterograde approach and also often limited by the size of the patients (Divers, 2015b).
Neoplastic lesions in rabbits are becoming more common because the extended lifespan of the patients and the better diagnostic and treatments available (Bertram et al, 2021).
Osteoblastic osteosarcoma is the type of sarcoma most commonly described in rabbits (Ishikawa et al, 2012), and the neoplastic behaviour is prevalent malignant, with metastasis often present by the time of diagnosis (Zeeland, 2017).
In rabbits, osteosarcoma seems to affect more the axial skeleton, with preference for the skull and facial bones (Zeeland, 2017; Baum, 2021; Bertram et al, 2021).
In this case, no metastases were evident on the CT scan, but the neoplasia was expanding through the cranium base already. Occasionally, extra-skeletal locations have been also reported (Wijesundera et al, 2013).
The affected anatomic areas vary for rabbit osteosarcoma compared to dogs and cats, where osteosarcoma represents up to 85% of osseous neoplasia (Ehrhart et al, 2013); about 75% of the cases affect the appendicular skeleton in dogs, while more contradictory data exist for cats (Ehrhart et al, 2013).
Metastasis of this neoplasm appears common by the time of diagnosis (Zeeland, 2017). In this case, no metastases were evident on the CT scan, but the neoplasia was already expanding through the cranium base.
The rationale for surgery was to improve airway diameter and to allow an improvement of the patient’s clinical status, which was deteriorating rapidly. The mass was occluding more than 90% of the available diameter of the retro-pharyngeal space (Figure 7).
The decision to proceed concurrently with the incisor extraction, specifically requested by the owner, was made because of the stable anaesthetic and the short time spent to debride the retro-pharyngeal neoplasia.
Unfortunately, despite an uneventful recovery from the procedure and the improved respiratory patterns, the patient’s general conditions failed to improve and, during the first postoperative check done three days after the discharge, the rabbit’s general status declined and a suspected failure of the suture of the surgical area happened, possibly worsening the situation.
The generalised deterioration of clinical conditions could be explained by the supplemental trauma of the incisors’ extraction or by the inflammation of the intra-cranial portion of the neoplasia after the debridement. Of more difficult explanation is the failure of the surgical site’s suture; in dogs and cats with oesophagostomy tube placement, the area does not need any suture after the removal of the tube and normally heals without complications (MacPhail et al, 2019).
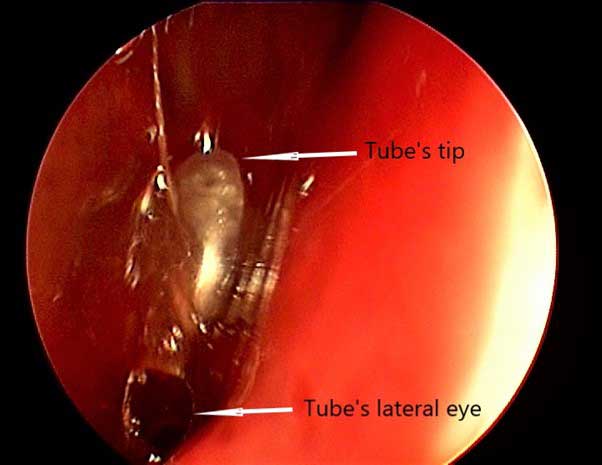
The procedure was tried on a cadaver rabbit of patient’s similar size to highlight the anatomic structures of the area and check the feasibility of the approach.
After the incision and the insertion of the endoscope through surgical opening, a nasogastric tube was inserted in one of the cadaver nostrils and the tip was easily visualised, confirming the correct positioning of surgical access (Figure 8).
The procedure was easy to perform and with numerous diagnostic and surgical possibilities for the access of an anatomic area difficult to access in rabbits due to the particular anatomy of the region. Unfortunately, the post-surgical complications should have been investigated further to understand if they were related to the procedure itself, or to the specific clinical condition of the patient.
- Thanks go to Halesowen College Animal Care unit for the use of the deceased rabbit to practice the technique, and to Daniela Denk and International Zoo Veterinary Group for the histopathology and bacteriology tests of samples, and to the whole staff of Manor Vets’ exotics department.
- Use of some of the drugs mentioned in this article is under the veterinary medicine cascade.
References
- Baum B (2021). Not just uterine adenocarcinoma – neoplastic and non-neoplastic masses in domestic pet rabbits (oryctolagus cuniculus): a review, Veterinary Pathology 58(5): 890-900.
- Benato L et al (2021). Rhinitis/sinusitis, rabbits, Vetlexicon, www.vetstream.com/treat/lapis/freeform/rhinitis-sinusitis
- Bertram CA et al (2021). Neoplasia and tumor-like lesions in pet rabbits (oryctolagus cuniculus): a retrospective analysis of cases between 1995 and 2019, Veterinary Pathology 58(5): 901-911.
- Divers SJ (2010). Exotic mammal diagnostic endoscopy and endosurgery, Veterinary Clinics of North America: Exotic Animal Practice 13(2): 255-272.
- Divers SJ (2015a). Making the difference in exotic animal practice the value of endoscopy, Veterinary Clinics of North America: Exotic Animal Practice 18(3): 351-357.
- Divers SJ (2015b). Rabbit rhinitis: a diagnostic approach, Tokyo Vets, www.tokyovets.com/2017rabbitresp1.pdf
- Eatwell K (2012). Approaches to nasal disease in rabbits, Vet Times 42(34): 18-19.
- Ehrhart NP et al (2013). Tumors of the skeletal system. In: Withrow and MacEwen’s Small Animal Clinical Oncology, Elsevier Saunders, St Louis, Missouri: 463-503.
- Ishikawa M et al (2012). Osteoblastic osteosarcoma in a rabbit, Comparative Medicine 62(2): 124-126.
- Lhermette P and Sobel D (2008a). Rigid endoscopy: rhinoscopy. In: BSAVA Manual of Canine and Feline Endoscopy and Endosurgery, BSAVA, Gloucester: 117.
- Lhermette P and Sobel D (2008b) Rigid endoscopy: rhinoscopy. In: BSAVA Manual of Canine and Feline Endoscopy and Endosurgery, BSAVA, Gloucester: 114-117.
- MacPhail C et al (2019). Nutritional management of the surgical patient. In: Fossum TW (ed), Small Animal Surgery (5th edn), Elsevier, Philadelphia: 97.
- Silvetti S (2021). Nasal adenocarcinoma: diagnosis and treatment in a pet rabbit (oryctolagus cuniculi), Vet Record Case Reports 10(1): 1-6.
- Varga M (2014). Abscesses. In: Textbook of Rabbit Medicine (2nd edn), Elsevier, Philadelphia: 256–257.
- Wijesundera KK et al (2013). Spontaneous extraskeletal osteosarcoma in a rabbit (oryctolagus cuniculus): histopathological and immunohistochemical findings, Journal of Toxicologic Pathology 26(3): 309-312.
- Zeeland YRA (2017). Rabbit oncology: diseases, diagnostics and therapeutics, Veterinary Clinics of North America: Exotic Animal Practice 20(1): 135-182.
Meet the authors
Lourdes Lavilla-Atienza
Job TitleSergio Silvetti
Job Title